What is Prior Authorization Process?
Insurance Companies are asking the providers to get approval or to take permission before rendering certain medical services. This is needed to ensure the medical necessity of the treatment rendered. Not all services require Prior Authorization, but a list of services that require prior authorization is being issued by every insurance.
The Utilization and Management Review department in the Insurance Company would issue the Prior Authorization. This process usually starts after verifying benefits. The process of obtaining authorization is simple, yet required so much attention and precise work. In case of emergency no authorization is required.

Importance of Authorization:
The Insurance Verification team plays a significant role and creates the base for the pre-authorization process. The Prior Authorization process helps providers to increase revenue as well as to reduce authorization related denials. If the claim is denied due to not having approved authorization in that case chances of getting payment for that service is become extremely less. Not taking authorization can lead to financial liabilities for both the patient as well as the healthcare provider. Therefore, having a partner like ingenious outsourcing to handle your medical billing and authorization process is the key towards increased reimbursement and eliminate adjustment or write off causing due to not obtaining authorization.
Authorization Request process at Ingenious Outsourcing:
There is total three ways to request authorization: over the phone, via web-portal, or by fax. It is completely depended upon insurance companies’ rules and guidelines. Ingenious outsourcing has a team of experienced Prior authorization team who understand the payor-based nuances to get the best out of them and ensure to have authorization on timely manner. It helps providers to submit claims with the approved authorization and get maximum reimbursement. We also follow a standard checklist of information and documentations required depending upon the payor and insurance policy, to avoid last minute hassle. Listed below are basic information that is standard across most insurance companies to submit an authorization:
Prior Authorization Process Flow
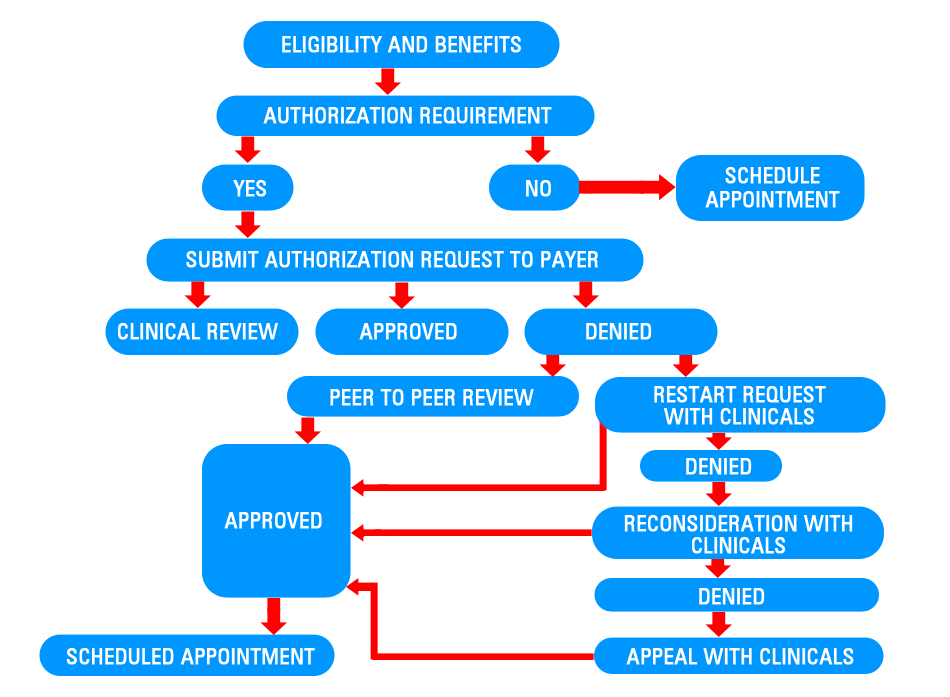
Under the umbrella of Authorization, we are not only help providers to obtain prior authorization, but we also provider related services like: PCP referral, Extending expired authorization, getting approval for additional units, and retro authorization.
The requirements of authorization may vary based on the insurance plan specific guidelines and place of service. In majority cases, risky and expensive treatments require prior approval from the insurance companies. So, the failure of obtaining authorization can lead big financial loss for providers.
- PCP referral is required for HMO plans. In addition, authorization request may result in the denial of an authorization request.
- Expensive service and risky services generally required prior authorization.
- Several insurance companies have health consultants like: Evicore, NIA, AIM specialty, American Health Group, etc. to handle authorization requests on their behalf.
- Outpatient emergency services do not require pre-authorization.
Ingenious outsourcing stick to the standard and proven process to help obtaining prior authorization well in advance to eliminate unnecessary denials.