In the ever-evolving healthcare landscape, provider credentialing and enrollment play a pivotal role in ensuring the delivery of quality care and financial stability for healthcare providers. Ingenious outsourcing offers comprehensive medical credentialing services, handling all necessary requirements, applications, and requested items. We guide providers throughout the process until they are enrolled and receive an effective date, approval letters, contracts, and fee schedules.

What is credentialing?
Provider credentialing in Medical Billing refers to the process of verifying and evaluating the qualifications and legitimacy of healthcare providers to ensure they meet the standards set by insurance companies, government agencies, and other healthcare organizations. In simpler word credentialing means process of verifying and assessing the qualifications, experience, and professional background of healthcare providers. It is an essential step to ensure that providers meet the stringent standards set by regulatory bodies, insurance companies, and healthcare organizations. Credentialing involves a meticulous evaluation of various aspects, including education, training, licenses, certifications, work history, malpractice claims, and disciplinary actions.
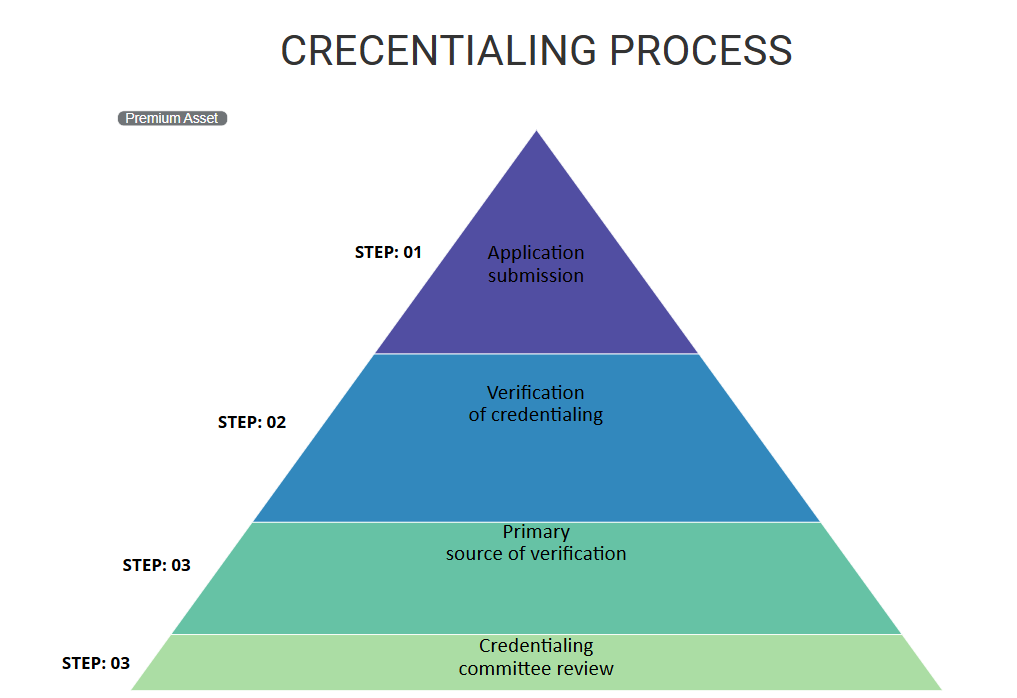
It’s a crucial step in the healthcare system to ensure that patients receive quality care from the qualified professionals and that healthcare providers can get reimbursed for their services. The actual process is very lengthy and time consuming. Here, is the breakdown of credentialing process in Medical Billing.
Healthcare providers, such as physicians, nurses, therapist and facilities like hospitals or clinics, submit applications to the insurance companies, government agencies, or managed care organizations to become approved providers within their network.
This is the step where detailed review of provider’s credentials, including their education, training, licence, board certification, work history, malpractice history, and any relevant accreditations, is taken place. This process ensures that the provider meets the required standards for delivering healthcare services.
This step involves confirming information directly from the original source, such as get in touch with educational institution, licensing board, and previous employers to verify the accuracy of the information provided by the healthcare provider.
A committee within the credentialing organization or insurance company evaluates the verified information and determines if the provider meets their standards and guidelines. This is where they approve or deny the application based on the completeness and accuracy of the given information.
Once the provider’s credentials are verified and approves, they are become in network provider with particular insurance company or healthcare organization. This step involves signing contracts that outline the terms of reimbursement, services provided, and other relevant details.
Credentialing is not one time process. Providers are re-evaluated after every certain time frame. Re-credentialing occurs at regular intervals, usually every one to three years, to confirm that provider continues to meet the required standards.
Apart from credentialing, some healthcare settings involve privileging, which grant specific clinical privileges to providers based on their credentials, experience, and training. For example, a hospital give permission to surgeon to perform surgeries after assessing their skills and experience in that particular area.
The credentialing process is very crucial for healthcare organizations, insurance companies, and patients. It helps maintain quality standards, ensures that patient receive care from competent providers, and allows providers to receive reimbursements for their services within the healthcare system.
There are several advantages of provider credentialing in Medical Billing. Here is the list of benefits.
CREDENTIALING VS ENROLLMENT:
Provider credentialing and provider enrollment are two distinct but interconnected processes in the healthcare industry. Provider credentialing refers to the comprehensive evaluation and verification of a healthcare provider’s qualifications, licenses, certifications, and professional background to ensure their competency and adherence to regulatory standards. It involves assessing a provider’s education, training, work history, and any disciplinary actions or malpractice claims. On the other hand, provider enrollment is the process of establishing a formal relationship between a healthcare provider and an insurance company. It involves completing the necessary paperwork, contracts, and agreements to become a participating provider in the insurance company’s network. While credentialing focuses on assessing qualifications and competency, enrollment focuses on establishing the contractual and administrative aspects necessary for a provider to receive reimbursement for services rendered to patients covered by the insurance company.

Most of the time people are considering medical credentialing and enrollment as one process. However, there is a significance difference between both of these processes. Let’s understand credentialing first. Credentialing is the process of verifying a provider’s qualifications and history through primary source verification. This process is the first and necessary step for providers to get contracted with healthcare insurance plans. Contracted providers are also known as in-network providers and are enjoy certain benefits that allow to prosper as a business. Generally, in-network providers are enjoying a steadier stream of patients. Patient always want to pay as little as possible and for that their best option to pay less out of pocket on their plan is to stick with providers recommended by the insurance company. Most of the times, contracted providers get preference over non-contracted providers or non-participating providers. In addition, in-network providers get paid a pre-decided / pre-fixed reimbursement rate based on their contract. Hence, it is eliminating uncertainty regarding pricing and payment.
But provider won’t be receiving all these benefits automatically after completing the credentialing process. That is where enrollment process comes in. Now, let’s understand what is enrollment. Provider enrollment is a crucial process carried out by insurance companies to establish a formal relationship with healthcare providers. It involves the thorough evaluation of a provider’s qualifications, licenses, certifications, and practice details to determine their eligibility to participate in the insurance company’s network. Insurance companies conduct provider enrollment to ensure that their network comprises competent and qualified professionals who meet the necessary standards of care. By completing the enrollment process, providers gain the opportunity to offer their services to a wider patient base covered by the insurance company, facilitating smoother billing and reimbursement processes. The process of enrollment follows the credentialing process. Once the provider is credentialed, they can enroll their practice or business for claims submissions and payment details like; EFT deposits, and EOB, or ERA. Enrollment needs to be completed at the time of billing setup and is usually done through third-party clearing houses.
What are the benefits you get if you outsourcing credentialing and enrollment process with Ingenious outsourcing?
Expertise and Experience: We have dedicated teams with in depth knowledge of credentialing requirements and the ability to navigate complex procedures. They ensure accurate and timely submission of applications, reducing the risk of errors and delays.
Time and Resource Efficiency: Aa a medical billing company, our goal of to make providers free from this complex process so they can focus on patient care. We ingenious outsourcing, are here to handle administrative tasks, including gathering and verifying documentation, following up on application statuses, and communicating with insurance companies and healthcare organizations.
Network Expansion: Ingenious outsourcing has established relationships with various insurance companies and healthcare organizations. By partnering with them, providers can access a broader network of payers, expanding their patient base and revenue potential.
Compliance and Updates: We as a Medical billing company always stay up-to-date with evolving industry regulations to ensure providers remain compliant with rules and regulations. We proactively monitor credentialing requirements, re-credentialing deadlines, and changes in insurance networks, reducing the risk of lapses in coverage.
Standard document: We have created special documents which gives you all your enrollment and credentialing related details. It includes, insurance name, enrollment date, future re-credential date, track record of credentialing and enrollment application. All your credentialing and enrolllment details are available at one place.
To summarise, provider credentialing is a vital process that ensures healthcare providers meet the necessary qualifications and standards for delivering safe and effective care. By partnering with Ingenious Outsourcing, healthcare providers can streamline their credentialing and enrollment processes, allowing them to focus on patient treatment while ensuring timely reimbursement, enhanced professional reputation, and compliance with regulatory standards.